Trauma and addiction are two complex issues that frequently coexist, and their connection is frequently misunderstood or misdiagnosed. While many people believe that addiction is a choice or a moral failing, research has shown that it is a chronic and relapsing brain disease that is strongly linked to past trauma. In this article, we will look at the connection between trauma, addiction, and misdiagnosis, as well as how healthcare professionals can better recognise and treat these issues.
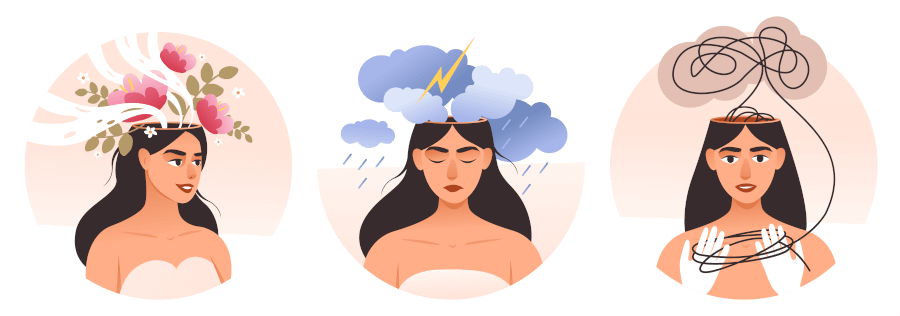
Trauma is defined as an overwhelming experience that exceeds an individual’s ability to cope. Physical or sexual abuse, neglect, violence, natural disasters, or accidents can all contribute to it. Anxiety, depression, flashbacks, nightmares, dissociation, hyperarousal, and avoidance are just a few of the physical, emotional, and psychological symptoms that can result from traumatic experiences.
Many trauma survivors turn to substance abuse as a coping mechanism. Drugs or alcohol can provide temporary relief from the traumatic memories, feelings, and sensations. Substance abuse, on the other hand, can lead to addiction, which is characterised by compulsive drug seeking and use despite negative consequences.
Trauma and addiction are strongly linked, according to research. The National Institute on Drug Abuse (NIDA) reports that up to 75% of people seeking substance abuse treatment have a history of trauma. Furthermore, trauma can increase the likelihood of developing addiction, as well as other mental health problems like depression, anxiety, and post-traumatic stress disorder (PTSD).
One of the difficulties in addressing trauma and addiction is the possibility of misdiagnosis. Many people seeking substance abuse treatment are not screened for trauma or other co-occurring mental health conditions. As a result, they may receive a diagnosis and treatment plan that focuses solely on their substance use and ignores underlying trauma or other issues.
A person who drinks to cope with the symptoms of PTSD, for example, may be diagnosed with alcohol use disorder (AUD) and treated with medication or behavioural therapy without addressing the underlying trauma. This method may provide short-term relief from alcohol cravings or withdrawal symptoms, but it does not address the underlying cause of the addiction or PTSD. As a result, the individual may be more likely to relapse or develop other problems in the future.
Attention-deficit/hyperactivity disorder (ADHD), which shares some symptoms with trauma and addiction, is another common misdiagnosis. People with ADHD, for example, may struggle with concentration, impulsivity, and restlessness, which can also be seen in people with PTSD or substance use disorders. Treating someone with ADHD medication without addressing trauma or addiction, on the other hand, can exacerbate the underlying issues and increase the risk of substance abuse.
To address the complex interplay of trauma, addiction, and misdiagnoses, healthcare professionals should assess and treat patients using a holistic and integrated approach. Screening patients for trauma and other co-occurring mental health conditions, as well as providing trauma-informed care that recognises the role of trauma in addiction and recovery, are all part of this.
In traditional treatment settings, trauma-informed care entails creating a safe and supportive environment that recognises potential triggers and re-traumatization. It also entails empowering patients to take an active role in their own treatment and providing them with options and alternatives that aid in their recovery.
Healthcare providers should consider evidence-based treatments that address both trauma and addiction, such as cognitive-behavioral therapy (CBT), dialectical behaviour therapy (DBT), eye movement desensitisation and reprocessing (EMDR), and trauma-focused CBT (TF-CBT). These therapies can assist patients in processing traumatic memories and developing coping skills, lowering the risk of relapse and improving overall mental health.
Misdiagnoses can prevent you from getting the help you need. We often find that post-traumatic stress disorder and complex post-traumatic stress disorder play a large role in the manifestation of an illness. Learn about the relationship between trauma addiction and how misdiagnoses can skew the picture and how this picture can become clearer when the right diagnosis is in place.
If you found this interesting you may also want to have a look at the full free video series on trauma based treatment models here.